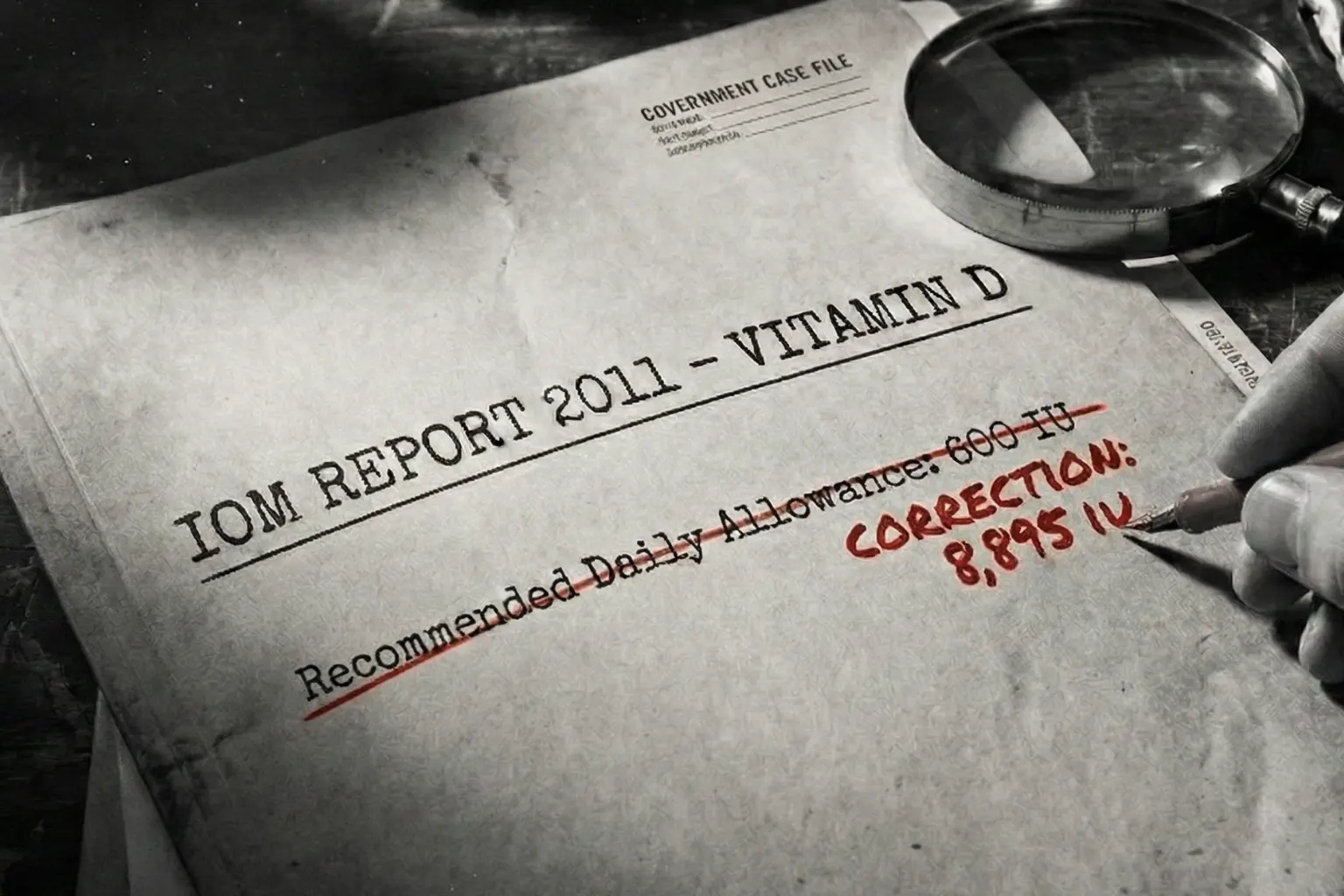
In 2017, the body responsible for setting Vitamin D standards in North America admitted that its flagship guideline was built on ‘material errors of calculation’.
The number stayed anyway. That decision left a global dietary rule in place that no longer matches the mathematics used to justify it.
Note: This is an audit of a government document, not a medical prescription. We are investigating a statistical error in the official record. We are not advising you to take 8,000 International Units (IU) of Vitamin D. The safety of high doses is still debated, and biological requirements vary by individual. Always consult a medical professional before changing your routine.
Where the 600 IU Vitamin D Number Came From
In 2008, the United States and Canadian governments asked the Institute of Medicine (IOM) to update the Dietary Reference Intakes for calcium and Vitamin D. The previous guidance, from 1997, predated most modern Vitamin D research.
The committee was chaired by Dr A. Catharine Ross and included clinicians, nutrition scientists, and statisticians drawn from both countries. The task was to specifically define the Recommended Dietary Allowance (RDA).
By definition, the RDA is a coverage threshold rather than an average. It is the daily intake intended to meet the needs of nearly all healthy people, defined quantitatively as 97.5 per cent of the population. That definition matters. It dictates the mathematics that must be used.
To anchor the recommendation, the committee chose a biological target. They decided that a blood concentration of 25-hydroxyvitamin D, written as 25(OH)D, of 50 nanomoles per litre was sufficient to protect bone health. 25(OH)D is the main circulating form of Vitamin D and the standard marker used in blood tests. Below that level, the risk of rickets and osteomalacia rises.
The next step was to work out how much oral Vitamin D intake was required to get people to that blood level. For this, the committee relied on ten supplementation trials conducted during winter at northern latitudes. Winter conditions were chosen to minimise Vitamin D made in the skin from sunlight, which would otherwise blur the intake–response relationship.
Those trials produced 32 study-level averages linking daily Vitamin D intake to achieved blood levels. To combine them, the committee used a mixed-effect regression model. In simple terms, this is a statistical method that allows results from different studies to be pooled while accounting for the fact that participants within the same study tend to behave more similarly than participants across studies.
The model produced a curve showing expected blood levels at different intakes. From that curve, the committee concluded that an intake of 600 international units per day would be sufficient to ensure that 97.5 per cent of people reached or exceeded the 50 nmol/L target.
That figure was published in January 2011 and rapidly became the regulatory standard. Once adopted, the number travelled far. It informed food labelling rules, school meal planning, military rations, and clinical advice given to patients with no diagnosed deficiency.
Timeline of the Vitamin D Standard
-
29 Sept 2008
Commission
IOM Committee tasked with updating the official standards for Vitamin D.
-
Jan 2011
Publication
IOM releases the official report setting the RDA at 600 IU.
-
Oct 2014
The Audit
Veugelers and Ekwaru publish findings identifying the statistical error.
-
May 2017
The Admission
NAM Phase I Panel confirms "two material errors of calculation".
The Statistical Error
In October 2014, two statisticians from the University of Alberta, Paul Veugelers and John Paul Ekwaru, revisited the 2011 calculation. They did not collect new biological data. Instead, they re-analysed the same intake–response evidence used by the Institute of Medicine.
Their objection focused on a single technical point with large consequences. The committee had used the variation between study averages to estimate how tightly individual responses clustered around the regression curve.
That variation is described by the standard error of the mean (SE). It tells you how precisely you know the average result of a study.
What the RDA requires is something else. To cover 97.5 per cent of individuals, you need the standard deviation (SD) of individual responses. That describes how spread out real people are around the average. In nutrition studies, the spread is wide. Some people need far more intake than others to reach the same blood level.
By using the variation of study means rather than the variation of individuals, the model effectively compressed the population. The curve looked much tighter than it should have. A dose that would reliably get the average participant to the target was treated as if it would also cover almost everyone.
This is not a subtle statistical preference. Prediction intervals based on standard errors answer the question ‘Where is the true average likely to lie?’. Prediction intervals based on standard deviations answer the question ‘Where will most individuals fall?’.
The RDA definition demands the second question.
Veugelers and Ekwaru pointed out that this choice made the lower bound of the prediction interval far too optimistic. The model implied that very few people would fall below the target at 600 IU. The underlying data did not support that claim. When they corrected the variance term, the picture changed immediately. The wide spread of individual responses reappeared, and the 600 IU line no longer sat safely above the threshold.
The Variance Error
Standard Error (SE)
Measures how accurate the average is. Used by IOM. Only covers the "average person".
Standard Deviation (SD)
Measures how different individuals are. Required for 97.5% coverage. Used by Audit.
The 8,895 IU Result
Using the same ten winter trials, Veugelers and Ekwaru recalculated the intake required to meet the stated goal. They kept the biological target fixed at 50 nmol/L. They kept the coverage goal fixed at 97.5%. Only the mathematics changed.
At 600 IU per day, the corrected lower prediction limit was not close to 50 nmol/L. It was about 26.8 nmol/L. This meant that under the official guideline, a substantial fraction of the population would remain in a range associated with deficiency.
To raise the lower prediction limit to the target level, the intake had to increase sharply. The corrected regression indicated that an intake of 8,895 IU per day was required to ensure that 97.5 per cent of individuals reached at least 50 nmol/L.
The size of the gap was striking. The official RDA and the mathematically derived requirement differed by a factor of nearly fifteen. This was not a rounding error or a conservative adjustment. It meant that the published recommendation could not, by definition, do what it claimed to do.
Other researchers reviewed the recalculation. In 2015, Robert Heaney and colleagues published a letter in the same journal agreeing that the statistical critique was valid. They reached the same conclusion. The original model answered the wrong question.
At this point, the issue was no longer a dispute between academics. The error went to the heart of how a national standard had been set.
The Calculation Gap
| Parameter | IOM 2011 Conclusion | 2014 Audit Correction |
|---|---|---|
| Statistical Basis | Mixed-effect model on study means | Regression on individual variance |
| Coverage Goal | 97.5% of population | 97.5% of population |
| Predicted Serum at 600 IU | > 50 nmol/L | 26.8 nmol/L |
| Required Dose (RDA) | 600 IU | 8,895 IU |
Confirming the Calculation Error
The National Academy of Medicine (NAM), which had replaced the Institute of Medicine as the operating body, convened an internal review in response to the criticism. In early 2017, it assembled a Phase I panel that included independent statisticians David Allison, Bhramar Mukherjee, and Suzanne Murphy.
The panel’s remit was narrow. It was asked to determine whether the calculations in the 2011 report were correct. It was not asked to rewrite the guideline or propose a new intake.
On 15 May 2017, the panel issued its findings. The language was careful but unambiguous. It confirmed that ‘two material errors of calculation had been made’ in the original report.
The first concerned the interpretation of data from a bone histology study by Priemel and colleagues. The original committee had calculated a joint probability across the sample rather than the conditional probability at a specific blood level. That misstep affected estimates of how many individuals were truly protected at the chosen threshold.
The second concerned the intake–response regression. The panel agreed that the model had failed to account properly for individual-level variability. As a result, the prediction intervals presented in the 2011 report were too narrow.
This confirmation mattered. It established, in the Academy’s own words, that the mathematics underpinning the RDA contained substantive flaws. The issue moved from external criticism to internal record.
...two material errors of calculation had been made...
National Academy of Medicine, Phase I Panel Report (2017)Why the RDA Was Not Revised
Having confirmed the errors, the Academy faced a practical question. Did those errors require the RDA to be revised?
To answer that, it convened a Phase II panel later in 2017. This panel reviewed the same material but was tasked with assessing the impact of the errors on the final recommendation.
On 15 November 2017, the panel issued its conclusion. It stated that the identified errors did not have a meaningful impact on the final RDA values.
The reasoning rested on a procedural claim rather than a statistical one. According to the Phase II report, the 2011 committee had not used the regression model deterministically to set the RDA. Instead, it had relied on collective expert judgement, considering the ‘totality of evidence’.
The graphs and equations in the report were described as supportive, not decisive. This position created a logical loop. The statistical analysis was presented in 2011 as the basis for the 600 IU figure. When that analysis was shown to be wrong, it was reclassified as illustrative.
The number remained after the mathematics used to justify it was reclassified as non-decisive. No alternative quantitative method was published to explain how expert judgement arrived at exactly 600 IU rather than 1,200 or 2,000. The record contains the conclusion, but not the decision rule that produced it.
The Logic Loop
IOM presents statistical model proving 600 IU is sufficient.
Audit proves model is flawed; correct maths requires 8,895 IU.
NAM declares statistical model "irrelevant" to final decision.
600 IU remains the standard based on "Expert Opinion".
The Review Panel Overlap
The composition of the review panels added another layer of tension. Documentation shows that Dr A. Catharine Ross and Dr Sue Shapses, both members of the original 2011 committee, participated in the 2017 review process.
This meant that individuals involved in producing the original calculations also took part in judging the significance of the errors in those calculations. In standard audit practice, such overlap would normally trigger recusal to preserve independence.
The Academy did not frame this as a conflict. It described the panel as balanced and expert. Even so, the arrangement blurred the line between review and self-assessment. The Phase II conclusion depended heavily on accepting that expert judgement outweighed the published mathematics. That judgment was rendered, in part, by the same experts whose work was under scrutiny.
The Review Panel Overlap
- Dr A. Catharine Ross: Chair of original 2011 Committee; Reviewer on 2017 Panel.
- Dr Sue Shapses: Member of original 2011 Committee; Reviewer on 2017 Panel.
The Toxicity Paradox
The refusal to revise the RDA created a second contradiction involving safety limits. Alongside the RDA, the 2011 report set a Tolerable Upper Intake Level, or UL, of 4,000 IU per day for adults.
The UL is defined as the highest daily intake unlikely to cause harm. To derive that figure, the committee identified a No Observed Adverse Effect Level (NOAEL) of 10,000 IU per day. This was the highest intake at which trials had not observed hypercalcaemia or other clear toxicity. To be cautious, the committee divided that figure by an uncertainty factor of 2.5, producing the 4,000 IU ceiling.
When placed next to the corrected adequacy requirement, a paradox emerges. The intake needed to ensure sufficiency for 97.5 per cent of people, 8,895 IU, lies well above the official safety limit.
Following the mathematics would require a dose labelled as potentially unsafe. The committee justified the conservative UL by citing observational studies suggesting U-shaped risk curves, where very high Vitamin D levels were associated with increased mortality. Critics have argued that these curves are artefacts of confounding and reverse causation, but the debate remains unresolved.
The result is a regulatory stalemate. Accepting the corrected RDA would force a reconsideration of the UL. Maintaining the UL requires dismissing the corrected RDA. The ‘expert opinion’ defence allows both numbers to stand without reconciling them.
Why the Number Still Matters
The decision not to correct the record has shaped guidance far beyond the Academy. Other bodies have had to choose whether to follow the 600 IU standard or depart from it.
The Endocrine Society, which issues clinical guidelines for treating patients, recommends daily intakes of 1,500 to 2,000 IU for adults to achieve blood levels above 75 nmol/L. Its approach focuses on individual optimisation rather than population minima.
Health Canada broke ranks in 2021. They raised the limit for over-the-counter supplements to 2,500 IU. That move suggests the fear of the 4,000 IU ceiling is fading, yet the official RDA used for federal programmes stayed exactly where it was.
The 600 IU figure still dictates the rules for food fortification and hospital meals. It survives because it is the path of least resistance. Correcting it would require tearing up the rulebook for multiple agencies at once.
The problem here is the bureaucracy, not the biology. A confirmed calculation error was identified, acknowledged, and then filed away as ‘irrelevant’. The standard stayed, and the advice followed it.
Authority Map
National Academy (NAM)
Admitted math errors but maintained standard based on opinion.
Health Canada
Raised supplement limit in 2021, diverging from NAM safety fears.
Endocrine Society
Treats individual sufficiency; ignores NAM population model.
Sources
Sources include: the 2011 Institute of Medicine report Dietary Reference Intakes for Calcium and Vitamin D, specifically the chapters establishing the 600 IU standard and the 4,000 IU safety limit; the pivotal 2014 audit ‘A Statistical Error in the Estimation of the Recommended Dietary Allowance for Vitamin D’ by Paul J. Veugelers and John Paul Ekwaru; internal National Academy of Medicine records comprising the ‘Phase I’ and ‘Phase II’ panel reports from 2017, which confirmed the calculation errors; the 2015 correspondence by Robert Heaney et al. validating the statistical critique; and comparative guidelines including the Endocrine Society’s clinical recommendations and Health Canada’s 2021 regulatory updates regarding supplement limits.
What we still do not know
- The Phase II Transcripts: We do not know the specific arguments used to dismiss the 8,895 IU calculation, as the meeting minutes are not public.
- The "Shadow" Methodology: If the regression model was irrelevant, the specific rubric used to arrive at exactly 600 IU remains unpublished.
- The Military Role: The Department of Defense sponsored the report. We do not know if they pressured for a conservative RDA to avoid the logistics of high-dose supplementation.
Comments (0)